- Jul 26
- 4 min
Electrocardiography - Part 2: Bradyarrhythmias
In Part 1 of this blog series on electrocardiography, we covered the basics of performing ECGs and looked at normal cardiac rhythms. Here we will explore the different types bradyarrhythmias and their corresponding treatments.
Sinus Bradycardia
A sinus bradycardia occurs due to decreased automaticity of the SA node, and can be recognized electrocardiographically when all criteria for sinus rhythm are present however the heart rate is considered bradycardic. Common causes of a sinus bradycardia include elevated vagal tone, heart-rate reducing drugs, sedation/anesthesia, and hypothermia, however hypothyroidism, athletic conditioning, hyperkalemia, and sinus node dysfunction (i.e., Sick Sinus Syndrome) can also contribute to this finding. Patients with intact sinus node function typically respond appropriately to anticholinergic therapy (i.e., atropine). In the absence of sinus node disease, treatment should be aimed at the contributing cause, if necessary.

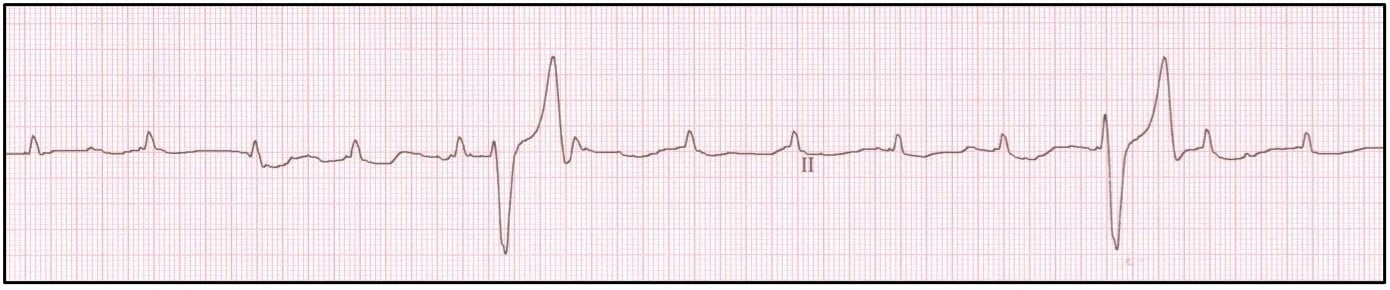
Sinus Node Dysfunction (Sick Sinus Syndrome)
Sick sinus syndrome (SSS) is used to describe a condition in which many different ECG abnormalities may be present indicating sinus node dysfunction. These typically include sinus arrest and/or sinus bradycardia, however even supraventricular tachycardia (SVT) can be present. Co-existing AV nodal dysfunction resulting in AV block is also common. Patients typically present for weakness, exercise intolerance, or syncope, however a surprising number of patients are asymptomatic. Sudden death is exceedingly rare in SSS patients. Patients presenting for syncope are typically affected with bradyarrhythmias, however concurrent tachyarrhythmias are possible (‘bradycardia-tachycardia syndrome’). Such patients can be difficult to manage as treatment for one rhythm disorder may exacerbate the other.
Sick sinus syndrome is almost exclusively recognized in canine patients, with Miniature Schnauzers, West Highland White Terriers, and Cocker Spaniels more commonly affected. The exact cause is unknown, however fibrous degeneration of the SA node and other cardiac conductive tissues is suspected.
Treatment of bradycardia associated with Sick Sinus Syndrome is dependent upon the clinical signs present (if any) and presence of concurrent tachyarrhythmias. Asymptomatic patients may require no treatment, while those with mild clinical signs may benefit from oral positive chronotropic therapy to help increase heart rate (i.e., terbutaline, theophylline, or hyoscyamine). Patients with severe bradycardia requiring hospitalization may require parenteral treatment (Atropine 0.02-0.04 mg/kg IV/IM/SQ, or isoproterenol 0.04-0.08 mcg/kg/min IV) prior to permanent pacemaker placement. Treatment of patients with ‘bradycardia-tachycardia’ syndrome often requires pacemaker placement for bradycardia which will allow for safe administration of anti-arrhythmic therapies for associated tachycardia. Treatment for SVT should not be performed in these patients unless pacing is available as such anti-arrhythmics will exacerbate bradycardia.
.jpg)
Did you know that Oncura Partners has a dedicated cardiology team that can review your ECGs? Click here to request more information about our electrocardiography support services.
Atrial Standstill
Atrial standstill occurs secondary to destruction of the atrial myocardium (typically due to fibrosis) or severe hyperkalemia. As a result, patients with this rhythm disturbance should always have serum potassium levels assessed. The ECG findings associated with this arrhythmia include a bradycardia with absence of atrial depolarization (no P-waves) and a junctional or ventricular escape rhythm.
In the absence of hyperkalemia, a diagnosis of atrial myocardial disease is inferred. With destruction of the normal atrial myocardium (also called ‘silent atrium’ or AV myopathy) the atrial musculature becomes unresponsive to SA nodal impulses with total absence of both atrial depolarization and contraction. Patients affected with AV myopathy may present for symptoms of bradycardia (lethargy, exercise intolerance, syncope) or congestive heart failure (pulmonary edema, ascites, pleural effusion). This unique disease is most commonly reported in the English Springer Spaniel, however other canine breeds and feline patients can be affected.
If hyperkalemia is present, emergent treatment of this electrolyte disturbance is advised as well as and any contributing cause (i.e., 0.9% NaCl, Calcium gluconate, insulin and dextrose containing fluids). In patients without hyperkalemia, treatment is aimed at increasing heart rate and controlling congestion, if present. This typically involves placement of a permanent pacemaker, however due to worsening fibrosis of the myocardium, progressive myocardial disease and symptoms of congestive heart failure is inevitable.
Atrioventricular Block
First Degree AV Block
First degree AV block is identified as delayed conduction through the AV node and is observed on ECG as a prolonged PR interval (PR interval > 0.13 seconds in dogs: > 0.09 seconds in cats). Although the electrical impulse takes longer to travel through the AV node, there remains synchrony of all P-waves to QRS complexes with first degree AV block. Causes typically include increased vagal tone, electrolyte disturbances, hypothermia, and various medications that can slow AV nodal conduction (i.e., digoxin, beta-blockers, Ca+ channel blockers, opioids). In some patients, recognition of this finding is indicative of emerging AV nodal disease. Treatment is typically not required, however periodic monitoring is beneficial if AV nodal disease is suspected.

Second Degree AV Block
Second degree AV block occurs when there is intermittent conduction through the AV node. As a result, some P-waves do not result in associated QRS complexes on the ECG however proper synchrony is maintained in those P-waves that are conducted. Causes can include high vagal tone, electrolyte disturbances, medications (i.e., digoxin, beta-blockers, Ca+ channel blockers, more rarely opioids), and AV nodal disease (i.e., fibrosis, myocarditis/endocarditis). The ratio of P-waves to QRS complexes gives an indication of severity (i.e., 4:1 block represents four atrial contractions for each ventricular contraction and is a ‘high-grade’ block relative to 2:1, as above). Assessment of remaining AV nodal function should include performance of an atropine response test. Similar to patients with SSS, patients with inherent AV nodal disease that are asymptomatic may require no treatment, while those with mild clinical signs may benefit from oral positive chronotropic therapy (Terbutaline 0.2 mg/kg PO q 8 12 h or Theophylline 10-15 mg/kg PO q 12 h). Patients with severe bradycardia requiring hospitalization may require parenteral treatment (Atropine 0.02-0.04 mg/kg IV/IM/SQ and/or isoproterenol 0.04-0.08 mcg/kg/min IV) prior to permanent pacemaker placement.

Third Degree AV Block
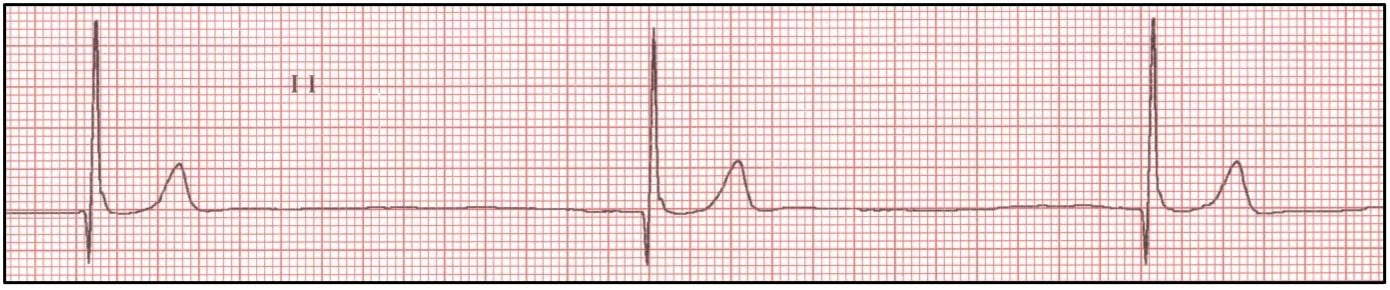
Third degree AV block is a complete dissociation of atrial to ventricular impulses. As a result, the patient's cardiac output is maintained by a junctional or ventricular escape focus. Given the substantially slower automaticity of the HIS-Purkinje system in canine patients (30-60 bpm), symptoms of decreased cardiac output are often present including severe lethargy, exercise intolerance, and syncope. Feline patients, however, rarely display overt clinical signs due to a more adequate ectopic pacemaker rate (90-130 bpm). Patients with long standing bradycardia may also develop severe myocyte stretch due to prolonged diastolic filling times, elevated ventricular filling pressures, and ultimately left- or right-sided congestive heart failure. Sudden death can also occur with cessation of impulse generation from escape foci. Possible causes of 3rd degree AV block are numerous including AV nodal degeneration or fibrosis, myocarditis, endocarditis, infiltrative heart disease, or an immune-mediated disorder.
Electrocardiographically, 3rd degree AV block appears as non-conducted P waves with a junctional or ventricular escape rhythm. It is important to recognize the life-saving function of the escape focus. Although ventricular escape complexes appear of similar morphology to ventricular premature complexes, ventricular anti-arrhythmic therapy (lidocaine, procainamide, mexiletine, beta-blockers, potassium channel blockers, etc.) is absolutely contraindicated. An isoproterenol CRI (0.04-0.08 mcg/kg/min) can be introduced as a temporary means to increase the ventricular response rate via stimulation of ventricular beta-adrenergic receptors, however permanent pacemaker implantation is preferred method of treatment. For patients that are unable to undergo pacemaker implantation, oral beta-agonists such as terbutaline can be attempted.