Ultrasound assessment of patients is extremely important in the acute veterinary setting. Point of care ultrasound (Global FAST) should be used in addition to thorough physical exam and laboratory evaluations to offer the timeliest diagnosis and therapeutic intervention in critical patients.
Ultrasound assessment of the gallbladder has proven to be an important tool. The finding of gallbladder wall edema (GBWE) in acutely ill patients can be a marker for anaphylaxis, right sided heart failure, pericardial effusion, or acute cholecystitis. Other documented causes include hypoproteinemia, immune-mediated anemia, pancreatitis, and post-transfusion (likely immune-mediated; possibly volume overload).
Here we will take a deeper look at the association between GBWE and anaphylaxis as seen in a recent case.
Presentation and Ultrasound Findings
An 18 month old F/I Yorkshire Terrier presented to the emergency room for acute onset of vomiting. Once arriving at the ER, her signs progressed with marked weakness, tachycardia, hypothermia, and hypotension. An initial “FAST” exam did not show any free fluid in her abdomen. She was admitted for fluid therapy and supportive care.
Laboratory findings: HCT 63%, platelet count 120,000; BUN 33 mg/dl, ALT 622 U/L, GGT 45 U/L; baseline cortisol normal; SNAP cPL abnormal; the next morning, chemistry profile showed albumin 2.0 g/dl, globulin 2.0 g/dl, ALT out of range, GGT 27 U/L.
The next morning an ultrasound was performed with the following findings: gallbladder wall edema, moderate volume peritoneal effusion (abdominal fluid score 4/4) and diffuse gastric changes (suggestive of non-specific gastritis).
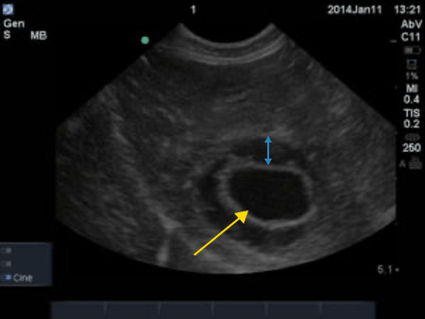
The yellow arrow points to the gallbladder. The blue double-sided arrow shows the thickened wall associated with the gallbladder halo sign.
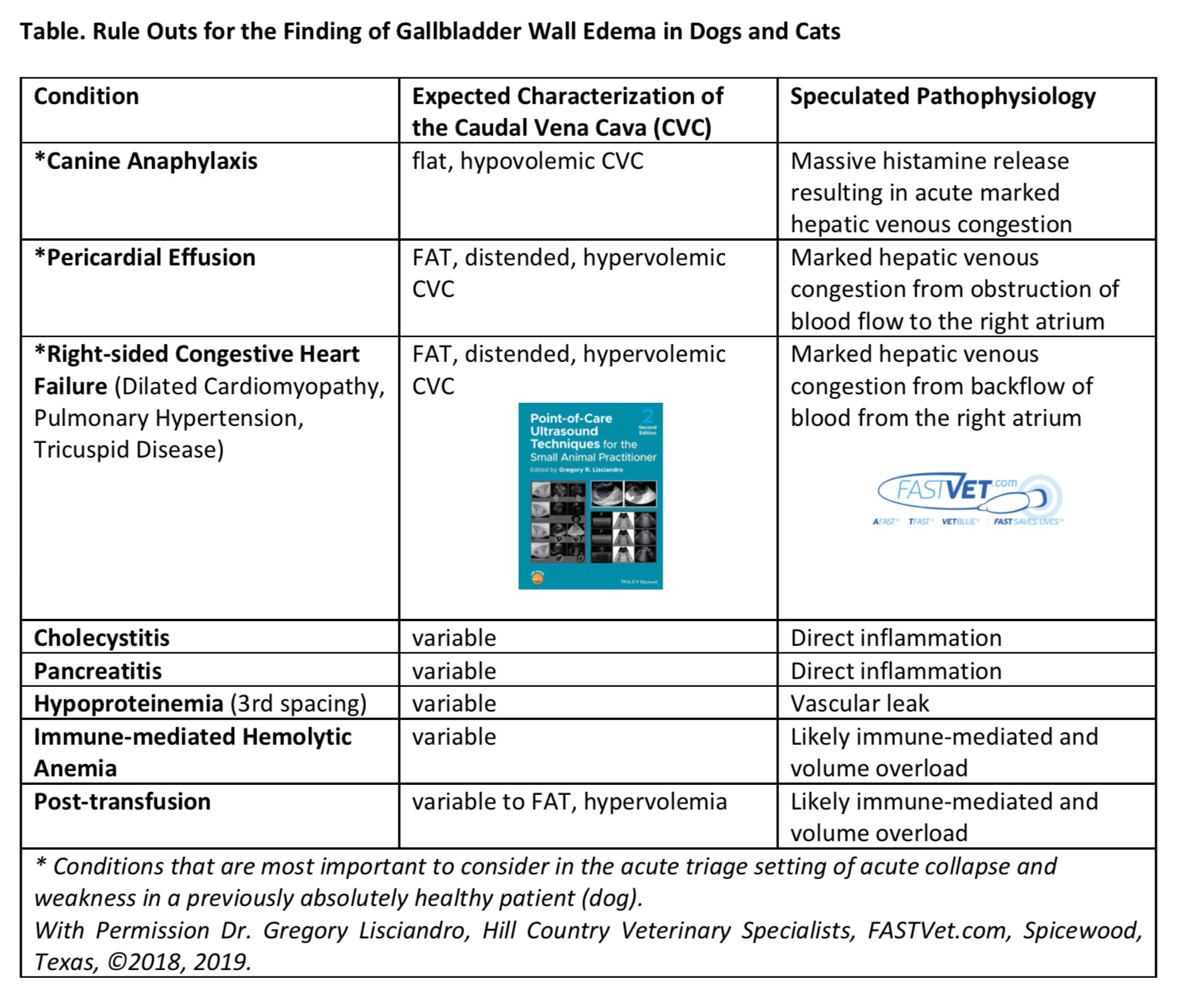
Gallbladder “halo sign” or wall edema is a non-specific finding. Considerations may include anaphylaxis, right sided heart failure, pericardial effusion (may be seen with tamponade), or cholecystitis among others (see chart below). Interpretation of this finding should always be done in conjunction with history and clinical signs. In this case, given the history, anaphylaxis was the primary consideration. It considered likely that the initial “FAST” exam did not follow a specified protocol but was rather a “Flash” of the abdomen and therefore, may have missed abdominal effusion. By following the standardized protocol of abdominal FAST (AFAST; Oncura teaches this standardized protocol), she was re-examined the next morning, and she had an abdominal fluid score of 4/4 which showed fluid at each standardized site. The primary consideration was anaphylaxis induced hemoabdomen. A coagulation profile was recommended and coagulation times were out of range.
How do we interpret gallbladder wall edema? It is important to be trained to evaluate the caudal vena cava which is visualized on images of liver (at the AFAST DH site). A “fat” vena cava with no bounce indirectly indicates elevated right atrial pressures and would be more consistent with right sided heart failure or pericardial effusion (this should lead you to evaluate the thoracic cavity for the cause of effusion). In this case, a “flat” vena cava (non-distended with no bounce) suggested hypovolemia. A flat vena cava in conjunction with gallbladder wall edema is suggestive of anaphylaxis especially with acute onset of signs as in this case.
In this case, she received fresh frozen plasma for her coagulopathy and was started on treatment for anaphylaxis including corticosteroids. She responded well and was discharged the next day.
Discussion: It is important to be able to recognize ultrasound findings in anaphylaxis to be able to treat the patient expediently. In this scenario, ultrasound can be truly life saving! Anaphylactic (AX)-related gallbladder edema is specific to canines because their shock organ is the liver and gastrointestinal tract. In contrast, the shock organ of cats and people is the lung, thus gallbladder wall edema is not a hallmark of AX in these species. Because the liver and gastrointestinal tract are the shock organs for the canine species, traditionally serum alanine transaminase (ALT) has been used as supportive evidence for canine AX. However, in the Quantz et al. study, it was stated that serum ALT marker was not as immediate as the occurrence of gallbladder wall edema; and that the ALT may not spike in value for up to 2-4 hours post-insult. The other important take home point in this case is that anaphylaxis may cause hemoabdomen and veterinarians should be aware of this fact. In general, after anaphylaxis is successfully treated, it should resolve ultrasonographically within 48 hours.
To learn more about using real-time, sonographer assisted veterinary ultrasound in your practice to quickly evaluate life-threatening conditions such as anaphylaxis, click here.