Pericardial effusion is a fairly common disease in dogs. In general, dogs with pericardial effusion present with weakness, collapse, or respiratory difficulty. However, dogs may have more general signs including inappetance, lethargy, exercise intolerance, or abdominal distention. The signs are especially difficult to detect in patients with chronic pericardial effusion. In addition, patients with chronic pericardial effusion may have physical exam findings that are non-specific and not be helpful in detecting the disease. In acute cases or patients with cardiac tamponade, signs may include distention of the jugular veins, muffled heart sounds, tachycardia, dyspnea, and poor pulse quality. Abdominal distention and ascites develop in patients with chronic disease.
In general, laboratory findings (results of CBC, chemistry profile, and UA) are non-specific. Patients may have mild anemia, neutrophilia or morphological changes of red blood cells (schistocytes, nRBCs, other). Chemistry profile may show elevated BUN/creatinine due to pre-renal azotemia because of decreased cardiac output. Coagulation profile should be performed to rule out coagulopathy
Thoracic radiographs may be insensitive in cases of acute pericardial effusion. Cardiac size may appear normal in acute cases since the pericardium has not had time to expand. In more chronic cases, the pericardium will expand and cause mild to moderate cardiomegaly (globoid heart). Other radiographic findings may include pleural effusion or distention of the caudal vena cava. Ascites is represented on abdominal radiographs by poor serosal detail and may be seen if the patient is in right-sided heart failure.
ECG generally shows sinus tachycardia. Electrical alternans (variable R wave amplitude) can also be seen, but the absence of electrical alternans on an ECG does not rule out pericardial effusion.
Echocardiography is the gold standard for the diagnosis of pericardial effusion. It should be noted that point of care ultrasound is a very effective tool for diagnosing pericardial effusion. The Global FAST protocol is a standardized point of care exam that can be performed in a standing position or right lateral recumbency with minimal stress on the patient.
The use of the Global FAST DH (Diaphragmatico-Hepatic) view is very sensitive for the diagnosis of pericardial effusion, a conclusion drawn from a recent retrospective study in the Journal of Veterinary Emergency and Critical Care (Lisciandro 2014). All patients with ascites should be examined at the DH view for pericardial effusion. As a telemedicine consultant, I often see patients that receive an abdominal ultrasound because they present with ascites and the clinician is examining the wrong body cavity (the effusion is due to heart failure or pericardial effusion). Use of point of care ultrasound or Global FAST will help direct imaging to the correct body cavity.
The use of the DH view, part of BOTH the abdominal FAST (AFAST) and thoracic FAST (TFAST) ultrasound formats, is advantageous for 2 major reasons:
- The acoustic window provided by liver and gallbladder is helpful and avoids air-filled lung which is problematic at transthoracic views.
- The muscular apex of the heart is much less likely to be confused with heart chambers (problematic at the transthoracic views). Because of the very short distance between the DH’s sub-xiphoid location and the apex of the heart, even small volume effusions of < 5 mm can be recognized via the DH view. See the image below.
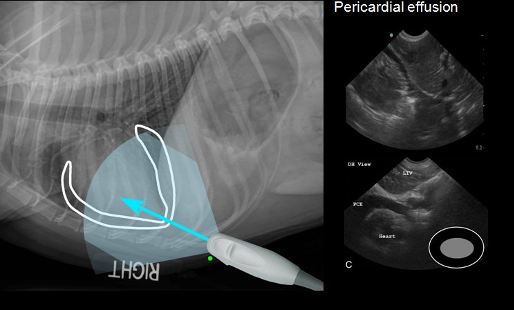
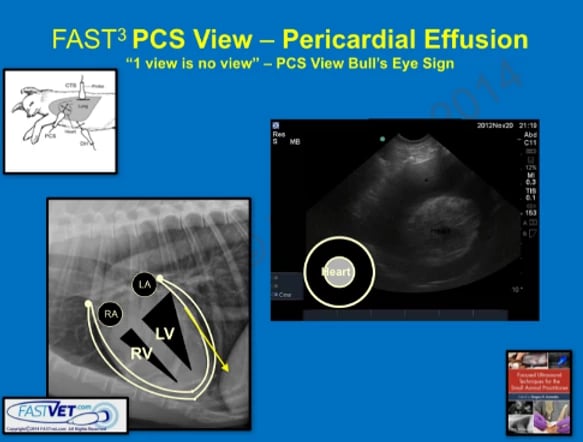
Image obtained from FASTVet.com (Copyright 2016)
To confirm pericardial effusion (PCE) that may be questionable at the DH view, additional views are recommended including the right parasternal short axis and 4 chamber long axis echo views. The right parasternal short axis view or “mushroom” view is obtained. We then recommend utilizing the imaging strategy of moving AWAY from the base of the heart and towards the apex of the heart to obtain the “bull’s eye” view.